Dental Implants 4 min read
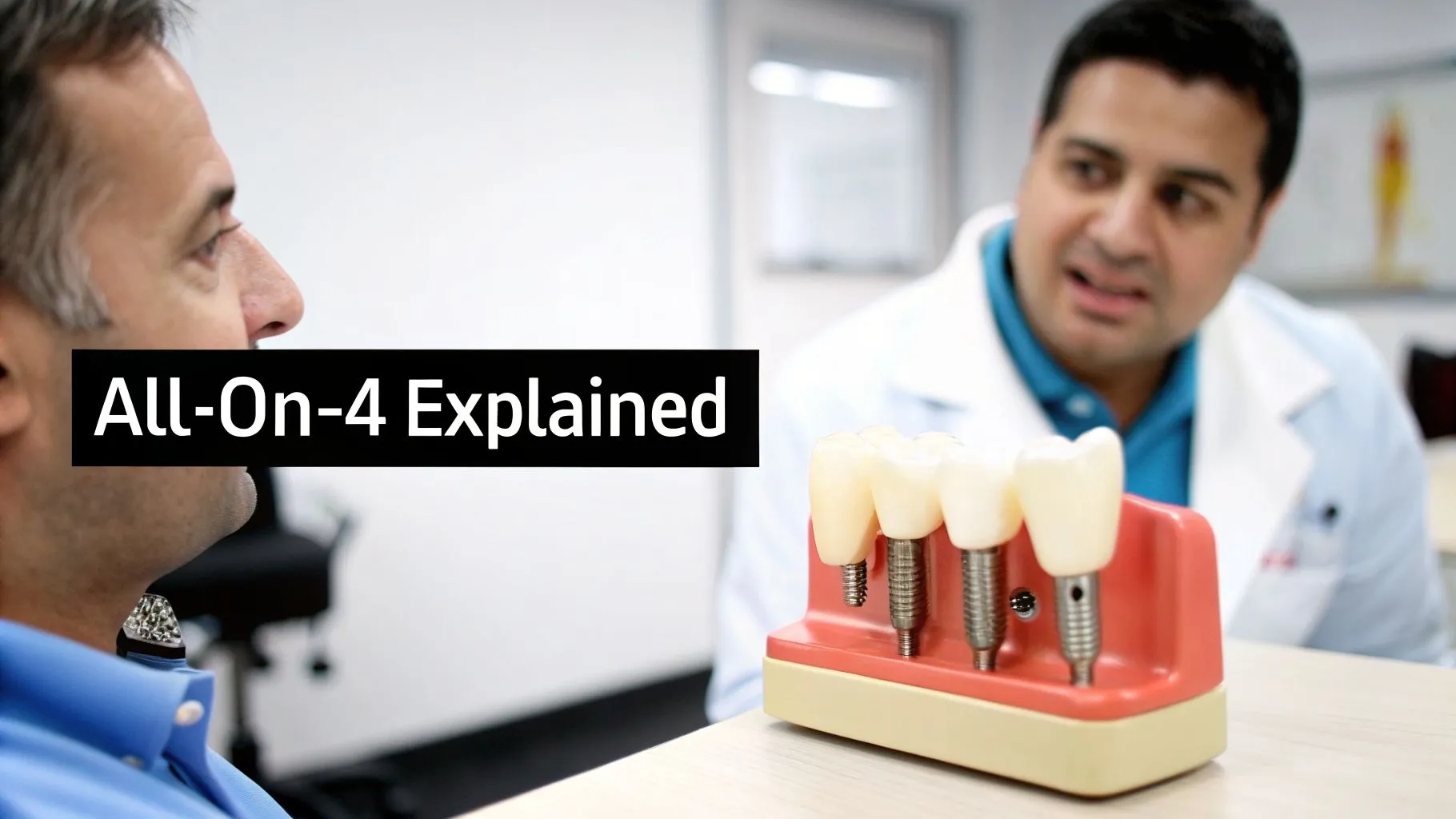
If you’re missing most or all teeth in one jaw, you usually don’t need an implant for each tooth. All-on-4 is for full-arch rehabilitation. Four implants go in planned positions. A fixed bridge sits on top. It restores appearance and function.
A key design feature is that the two posterior implants are typically placed at an angle. This approach can help use available bone more effectively and, in some cases, reduce the need for extra grafting. This depends on a clinical assessment.
All-on-4 at a Glance
| Feature | What it means for you |
|---|---|
| Full-arch restoration | Replaces an entire upper or lower arch |
| 4 implants | Efficient foundation for a fixed bridge |
| Angled posterior implants | Planned to maximise bone engagement in selected cases |
| Immediate function | A fixed temporary bridge may be fitted on the same day (case-dependent) |
| Structured treatment pathway | Diagnostics → digital planning → surgery → healing → final bridge |
Why Patients Choose All-on-4
All-on-4 is selected for stability, comfort, and day-to-day confidence. Compared with removable dentures, a fixed bridge can improve:
- Chewing stability (less movement, less reliance on adhesives)
- Speech confidence
- Comfort (reduced friction points from removable prostheses)
- Quality of life through predictable routines and follow-ups
Clinical outcomes vary. A detailed assessment (medical history + 3D imaging) is required to confirm suitability and risk profile.
“Teeth-in-a-Day” and Immediate Loading
One of the strongest value drivers of All-on-4 is immediate loading. In suitable cases, you may receive a fixed temporary bridge on surgery day.
This is not a marketing promise. It is a clinical decision based on primary stability, bone quality, bite factors, and overall health. When immediate loading is not advised, a staged approach can be planned for safety and predictability.
During healing, the implants go through osseointegration.
This is when the implant surface bonds with living bone.
It creates a strong base for the final restoration.
Who Is a Good Candidate?
All-on-4 is commonly considered for patients who:
- Have lost most or all teeth in one jaw
- Have loose, uncomfortable, or unstable dentures
- Want a fixed (non-removable) solution
- Have adequate bone volume/quality in key regions or are suitable for planned bone management strategies
Bone level and jaw anatomy
Bone resorption after tooth loss is common. The All-on-4 concept can be helpful because implant placement uses available bone. It often includes angled back implants when clinically appropriate.
General health factors that influence success
For implant surgery, we assess:
- Diabetes control (healing and infection risk management)
- Smoking status (higher complication risk; cessation protocols recommended)
- Bruxism (teeth grinding) (may require protective night guards and bite planning)
- Active gum disease (must be stabilised before implant rehabilitation)
When All-on-4 may not be appropriate
All-on-4 may require additional preparation or a different plan if there is:
- Uncontrolled systemic condition(s) affecting healing
- Active, untreated periodontal infection
- Severe parafunction (unmanaged bruxism)
- Complex anatomical constraints (confirmed by 3D imaging)
Your All-on-4 Treatment Journey (Step-by-Step)
1) Consultation & Diagnostics
We start with a structured consultation and clinical examination. For precision and safety, a 3D CBCT scan is often used. It checks bone volume, density, and nearby structures like nerves and sinuses.
2) Digital Treatment Planning
Using your 3D imaging, your clinician plans implant positions digitally. This improves:
- Predictability of implant placement
- Prosthetic design accuracy (smile line, bite relationship, aesthetics)
- Risk management (clearance from sensitive structures)
3) Surgery Day
On the day of surgery, the clinical pathway may include:
- Removal of failing teeth (if present and indicated)
- Implant placement according to the digital plan
- Fitting of a fixed temporary bridge when clinically appropriate
4) Healing & Osseointegration (Typically 3–6 months)
A structured healing protocol is followed. The temporary bridge supports aesthetics and function while protecting surgical sites with diet and hygiene guidance.
5) Final Bridge (Permanent Restoration)
After integration is confirmed, a final bridge is designed and fitted. Material selection depends on bite forces, aesthetics, and long-term maintenance goals (e.g., zirconia-based solutions when indicated).
Safety, Risks, and How Risk Is Reduced
Every surgical procedure has risks. In implant dentistry, common risks include infection.
They can also include injury to nearby structures.
Some people may have nerve symptoms.
Others may have sinus problems in the upper jaw. Mechanical problems can also occur, such as loose screws.
How we reduce risk (typical safeguards):
- 3D CBCT-guided planning
- Sterile surgical protocol and controlled clinical workflow
- Case-appropriate loading strategy (immediate vs staged)
- Structured follow-ups and hygiene support
If you have ongoing numbness, worsening pain, fever, or increasing swelling after early recovery, seek care right away.
Recovery & Aftercare (Practical Expectations)
First 72 hours: swelling and discomfort are common; instructions and medication protocols are provided.
First 2 weeks: soft diet and careful hygiene routines are prioritised.
3–6 months: integration phase; follow-ups confirm healing and stability.
Long-term: professional maintenance appointments + daily home care (bridge-under cleaning tools) are essential.
Your bridge can’t “get cavities,” but the gum and bone health around implants is critical for longevity.
All-on-4 vs Other Options (Clear Comparison)
Removable dentures: non-surgical, lower entry cost, but may be unstable and do not stimulate bone.
Conventional full-arch implants (often 6–8 implants): This is a fixed solution with excellent outcomes. It may need more bone and more complex grafting or surgery.
All-on-4: A fixed full-arch solution using fewer implants and planned placement. It often suits many cases after diagnostics.
Cost Drivers (Transparent, Non-Speculative)
All-on-4 pricing is case-specific. The main cost drivers typically include:
- Bone condition and need for adjunct procedures
- Complexity (extractions, infection management, bite rehabilitation)
- Bridge material and laboratory scope
- Digital planning and surgical approach
- Follow-up and maintenance plan
What to ask for (to ensure clarity):
- What is included in the package (diagnostics, surgery, temporary bridge, final bridge, follow-ups)?
- Implant brand and documentation
- Warranty/guarantee scope and conditions (implant vs prosthesis)


